Signs And Symptoms Of Baker Cysts
Baker cysts may be asymptomatic but become noticeable when they become swollen . Compression of adjacent tissue may cause pain usually with extension of the knee. Patients complain of worsening pain, increased knee stiffness, and decreased range of motion as the cyst becomes larger. Cysts can rupture, simulating deep vein thrombosis, with swelling, redness, warmth, and/or Homan sign.
What Are The Symptoms Of A Bakers Cyst
Sometimes youll feel no pain at all, or only a slight pain with a Bakers cyst. You may only have knee pain from the initial damage that caused the Bakers cyst, but not the lump itself. Any strain can cause this lump or your knee to swell in size. When the knee or cyst swells, this can increase your pain and limit how much you can move your knee.
Symptoms of a Bakers cyst may include:
- A fluid-filled lump behind your knee.
- Limited range of motion and ability to bend your knee.
- Swelling of your knee and/or leg.
Sometimes, a Bakers cyst can cause swelling and redness in your lower leg that can be similar to the symptoms of a blood clot. A blood clot is an emergency situation. If you are ever in doubt, reach out to your healthcare provider right away. Your provider can check out your symptoms and determine if its a Bakers cyst or a blood clot.
How Are Bakers Cysts Diagnosed
If your rheumatologist suspects you may have a Bakers cyst, they will likely start by asking about your symptoms. They may perform a physical exam, closely examining your knee for signs of inflammation and swelling. Although common in RA, Bakers cysts may elude clinical detection. For this reason, ultrasound imaging is often used to diagnose them. These scans produce highly detailed images of the area and can be used to rule out other causes of swelling, such as a tumor or blood clot. Your doctor may also recommend an X-ray or MRI.
You May Like: Bake Me A Wish Promo Code
What Is A Bakers Cyst
A Bakers cyst, also known as a popliteal cyst or synovial cyst, is a soft, fluid-filled lump that forms on the back of your knee. Like many diseases and disorders, this cyst is named after the doctor who first described it. In the mid-1800s, Dr. William Morrant Baker concluded that these popliteal cysts resulted from fluid flowing out from a damaged knee joint. When structures in or around the joint are damaged, your knee produces extra fluid that can only flow one way so it forms a cyst on the back of your knee.
Rheumatoid Arthritis Baker’s Cyst And Thrombophlebitis
Rheumtology Section, Veterans Administration Hospital, Ann Arbor, Michigan
Assistant Professor of Internal Medicine, University of Michigan Medical Center, Ann Arbor, Michigan
Rheumtology Section, Veterans Administration Hospital, Ann Arbor, Michigan
Assistant Professor of Internal Medicine, University of Michigan Medical Center, Ann Arbor, Michigan
From a small series of patients hospitalized with rheumatoid arthritis, six cases are presented in which Baker’s cysts were associated with pain and swelling of the calf, initially erroneously diagnosed as thrombophlebitis. The pathogenesis of these calf symptoms is reviewed.
Also Check: Honey Baked Ham Hickory Nc
What Are Possible Complications Of A Baker’s Cyst
The symptoms of a Bakers cyst are mild usually, however sometimes complications can develop, such as:
- the cyst continues to grow, causing your symptoms to worsen
- the cyst extends down into your calf muscles
- the cyst bursts, leaking fluid into the calf region, typically causing increased pain and bruising around the ankle.
If you experience any swelling or warmth in your calf, seek medical advice quickly.
It can be difficult to tell the difference between the complications of Bakers cyst and more serious problems such as a blood clot in the vein. So its better to be safe and get it checked out.
How Is A Bakers Cyst Diagnosed
You need a professional medical exam to diagnose a Bakers cyst. During your appointment, your healthcare provider may do several tests to both confirm the Bakers cyst and figure out what might be causing it, including:
- Taking a medical history: Your healthcare provider will ask you about any previous injuries you may have had to your knee and go over your entire medical history.
- X-ray: This test wont necessarily show the Bakers cyst itself, but it can be used to see if you have arthritis in your knee. Arthritis is one of the possible causes of a Bakers cyst.
- Magnetic resonance imaging scans: An MRI uses magnetic waves instead of X-rays to show detailed images inside the body. This test can give your provider even more information about what might be causing the Bakers cyst.
- Ultrasound: A simple and painless test, an ultrasound uses sound waves to determine if the lump is solid or fluid.
You May Like: Glenn Baker Heating And Air
What Causes A Baker’s Cyst
Knee damage caused by a sports injury or a blow to the knee can lead to a Baker’s cyst developing.
A Baker’s cyst can also sometimes occur if you have a health condition such as:
- osteoarthritis usually caused by age-related “wear and tear” of joints it particularly affects the knees, hips, hands and big toe
- inflammatory arthritis including rheumatoid arthritis, which is a less common type of arthritis and is caused by the immune system attacking the joints
- gout a type of arthritis that usually affects the big toe and is caused by a build-up of the waste product uric acid in the blood
Baker’s cysts usually develop in people aged 30 to 70, although they can affect people of any age, including children.
Physiotherapy Treatment Of Popliteal Cyst
Immobilization:
Immobilization is recommended for several weeks after surgery to immobilize the knee, this can be achieved by wearing a knee brace.
Strengthening exercises like quadriceps, hamstring, and gluteus medius strengthening are essential as their weakness can lead to poor knee biomechanics and cause pain and instability. Strengthening with weights can be limited initially to a pain-free range of motion, for this manual resistance, therabands and weight cuffs can be used.
Stretching exercises:
Stretching exercises are used to enhance the flexibility of the lower limb. Stretching of the hamstring, quadriceps, patellar ligament, and of other structures around the knee are recommended.
Don’t Miss: Baker City Motels And Hotels
What Is The Link Between Baker’s Cysts And Psa
PsA is a persistent inflammatory infection that occurs in people with psoriasis. PsA attacks joints and places where ligaments and tendons join to the bones in your body, such as the knees. The condition may appear at any age, including in childhood. It usually affects people ages 30 to 50, around 10 years after they developed psoriasis.3
If you have an existing issue with your knee, like PsA, you are more likely to develop a Baker’s cyst than people who do not. Osteoarthritis and rheumatoid arthritis also are often linked to Baker’s cysts.4
Diagnosis Of Baker Cyst
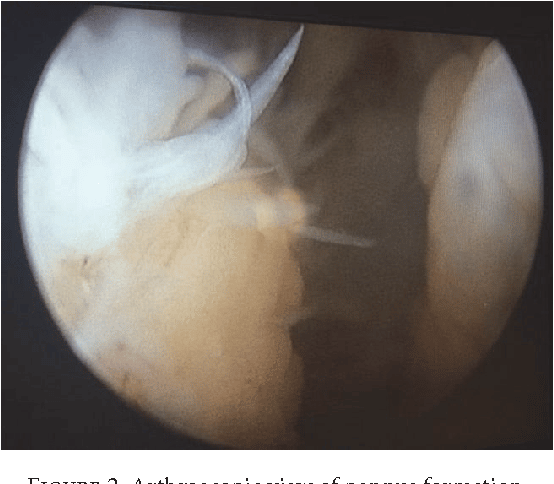
-
Sometimes, ultrasonography
-
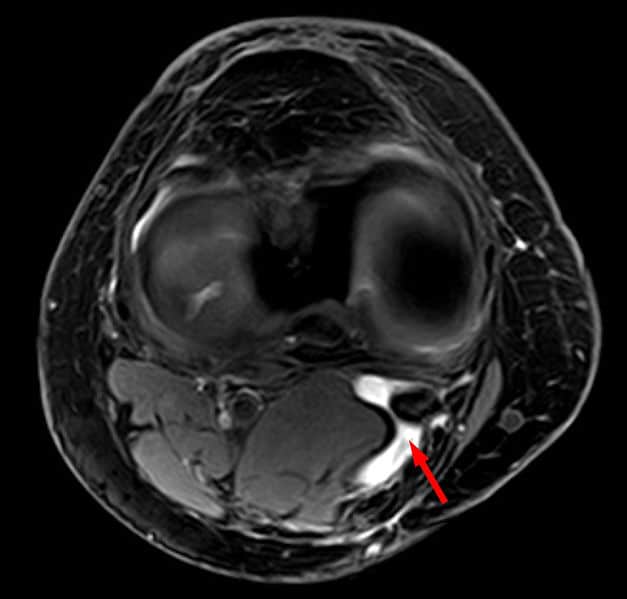
Sometimes, magnetic resonance imaging
Baker cysts are in the popliteal fossa. The cysts are more prominent and firm when the patient is standing and the knee is fully extended.
If clinical findings are inconclusive , ultrasonography can be done. Magnetic resonance imaging is done occasionally, eg, if ultrasonography is inconclusive or to diagnose and characterize internal knee derangements that may require surgery.
Don’t Miss: Ted Baker Card Holder Mens
Popliteal Cyst Or Miscellaneous Bursal Aspiration/injection
A popliteal cyst or other bursa, such as the pes anserine bursa, can be aspirated easily utilizing image guidance. Real-time ultrasound guidance is preferable because sonography allows one to confirm the presence of the fluid-filled cyst and also provides precise localization of the needle position during insertion . Popliteal cyst aspiration or other bursal aspirations can be performed for therapeutic purposes to relieve tension and discomfort associated with large popliteal cysts or inflamed bursae.20 Aspiration can also be performed for diagnostic purposes to identify the constituents of the fluid and evaluate for infection.20 Injection of anesthetic agents and steroids following aspiration can also be performed for therapeutic purposes. Unfortunately, pain relief following aspiration tends to be short in duration because popliteal cysts tend to recur quickly as a result of the persistent communication between the cyst and the knee joint.22,23
Darren C. Rosenberg DO, Joao E.D. Amadera MD, PhD, in, 2020
Does Immunoglobulin Help Keep Osetoarthritis At Bay

Q) I was diagnosed with osteoarthritis in my spine about 15 years ago. In 2000, I had Guillain-Barre syndrome and was treated with immunoglobulin. For many years my symptoms improved I’m wondering if the immunoglobulin helped to keep the osteoarthritis at bay and if it’s known that it does, why it isnt offered as a treatment?
A) Immunoglobulin is used for various rheumatic diseases. Generally it’s used for the connective tissue diseases, such as lupus, dermatomyositis and sometimes as emergency treatment where drugs which suppress the immune system can’t be used. It’s not known exactly how it works but it’s probably by several different mechanisms acting on the immune cells which are causing the problem. Although low-grade inflammation is seen in most joints affected by osteoarthritis it is, on the whole, a non-inflammatory problem and immunosuppressive drugs are seldom used. However, some people with osteoarthritis feel improved when they take drugs such as steroids and I think it’s for a similar reason that you felt better after these drugs. I’m assuming, however, that steroids weren’t part of your treatment regime when you had Guillain-Barre syndrome.
This answer was provided by Dr Philip Helliwell in 2011, and was correct at the time of publication.
Also Check: Best Degreaser For Baked On Grease
What Can I Expect From A Baker’s Cyst
Q) I have a Baker’s cyst on my right knee because of osteoarthritis. What am I to expect? How long will it last? Will I need a new knee eventually? Ive already had two hip replacements, so I use a crutch when I walk outside.
Rowena – 2017
A) A Baker’s cyst is a swelling that can develop behind the knee. It’s filled with synovial fluid, which is the lubricating fluid that’s usually found inside the knee joint. It most commonly occurs if there’s an underlying problem with your knee, such as osteoarthritis. A Bakers cyst often causes no symptoms, but some people can experience pain, swelling and tightness behind the knee.
Having a Bakers cyst doesnt necessarily mean you’ll need a knee replacement. Often it’ll get better on its own and the swelling goes away over time. In a small minority of people, they can split open and the fluid inside can leak out into the calf muscle, which causes swelling, redness and itching. If anything like this happens, you should get it checked out by your GP, as they’ll need to make sure that the symptoms are due to the Bakers cyst and not a deep vein thrombosis , which can cause similar symptoms, but needs treatment. However, most people with a Bakers cyst wont experience this.
This answer was provided by Dr Tom Margham in 2017, and was correct at the time of publication.
Is Chronic Inflammatory Arthritis The Same As Rheumatoid Arthritis
Q) I’m 63 and have suffered from osteoarthritis for around 10 years. I’ve recently been diagnosed with chronic inflammatory arthritis, at which time my consultant also used the words rheumatoid arthritis. Although the blood markers were negative, which he said applied to around 30 per cent of sufferers, an MRI showed inflammation and degeneration around the joints of my hands. He’s prescribed methotrexate and folic acid. Are these conditions the same? I’d like to refer to my condition correctly.
Nigel, Horsham, East Sussex – 2011
This answer was provided by Dr Philip Helliwell in 2011, and was correct at the time of publication.
You May Like: Where To Sell Baked Goods
Etiology Of Baker Cysts
Most Baker cysts accumulate fluid from the adjacent knee joint space. Increased synovial fluid production is caused by underlying joint disease. Synovial fluid flows from the joint toward the cyst with extension of the knee. Baker cysts can develop without knee joint communication in children.
Baker cysts are commonly caused by
-
Prior knee injury
-
Overuse of the knee
Diagnosis Of Popliteal Cyst
Physical examination:
The patient is asked about their medical history and previous knee injury. The patient is asked to describe symptoms. Then a physical examination of the affected knee is done and compared to the normal knee. The patient is examined for swelling, joint instability, clicking or popping noise when the knee is bent, joint stiffness and limited range of motion, etc. Palpation of the back of the knee is done where the cyst is located. Often, a cyst becomes firm when the knee is fully extended and soft when the knee is bent.
X-rays:
X-rays help to provide images of dense structures, such as bone. Although the cyst cannot be seen on an x-ray, the doctor can check for narrowing of the joint space and other signs of arthritis in the joint.
An ultrasound test uses sound waves to create images of structures inside the body. An ultrasound helps to look for the lump behind the knee and check whether it is solid or filled with fluid.
Magnetic resonance imaging scans:
Magnetic resonance imaging , is done to produce clear pictures of the body’s soft tissues. MRI scan shows an area of fluid behind the knee and the location of a popliteal cyst.
Recommended Reading: Baker’s Grocery Store Jobs
Ask The Doctor: How Do You Treat A Baker’s Cyst
- By Celeste Robb-Nicholson, MD, Contributor
Q. I have a Baker’s cyst in my right knee. It has been drained twice and recurred. Are there any other treatments for it?
A. Your situation is fairly common. A Baker’s cyst is a fluid-filled sac that can develop in the popliteal space, the hollow at the back of the knee joint. It’s named for William Morrant Baker, a 19th-century surgeon who first described the condition. The cyst is filled with synovial fluid, a viscous material that lubricates the knee joint, reducing friction among the components of the joint and allowing the knee to flex and extend freely. There are several ways to treat a Baker’s cyst, but it will often recur if the underlying cause hasn’t been addressed.
A Baker’s cyst may occur as a result of an injury to the knee, such as a tear in a meniscus, or damage to the cartilage from conditions such as rheumatoid arthritis or osteoarthritis. These conditions may cause the synovial cells lining the knee joint to produce excess fluid. If the fluid bulges into the popliteal space, a cyst can develop . The excess fluid can also cause the whole knee to become swollen.
|
Baker’s cyst A Baker’s cyst forms when excess synovial fluid bulges into the hollow at the back of the knee joint. |
If cyst is related to knee arthritis, doctors often do a cortisone injection into the knee to reduce inflammation. Sometimes, a Baker’s cyst needs to be drained by a doctor experienced in this procedure..
Treatment For Rheumatoid Arthritis
Treating a Bakers cyst often involves treating the underlying cause of the cyst in this case, rheumatoid arthritis. There are several types of treatments for RA, including oral medications, injections, surgery, and lifestyle changes like diet and exercise. You and your rheumatologist can work together to find the right treatments for you.
Also Check: Where Can I Watch Murder She Baked
Does Rheumatoid Arthritis Contribute To Dry Eyes
Q) I’ve suffered from dry eyes for a long time. I suffer from rheumatoid arthritis and had a hip replacement in 2000. I’ve tried all the remedies the NHS has to offer and have been on sulfasalazine and methotrexate for three years. Does rheumatoid arthritis contribute to dry eyes? Can you suggest a cure or anything to relieve the symptoms?
Gordon, Shetland – 2010
A) Dry eyes are a recognised feature of rheumatoid arthritis. The rheumatoid process can cause damage to the cells that produce the moisture for the eyes and mouth. This is called Sjögrens syndrome . At its most severe, this condition can lead to damage of the surface of the eye and visual impairment, so it’s important to seek help. Mostly, lubricant eye drops are used, but sometimes surgical solutions are necessary. These include putting a plug in the duct that drains the tears away. Lubricants can also be used for the mouth and a tablet called pilocarpine may help both eyes and mouth.
This answer was provided by Dr Philip Helliwell in 2010, and was correct at the time of publication.
Can You Have Both Palindromic Arthritis And Rheumatoid Arthritis
Q) I was very interested in the article about palindromic rheumatism and felt that after 25 years of pain, disability and frustration I was finally reading something which explained my symptoms.
I had two years of flare-ups in my joints before getting a positive rheumatoid arthritis blood test. Over the years I’ve had longer term swelling in joints which have led to damage. However, the pain and pattern is totally different to the original flare-ups.
Over the years I’ve continued to suffer the flare-ups regularly while blood tests show the rheumatoid arthritis to be largely under control with methotrexate. I spoke to my nurse about a diagnosis of palindromic rheumatism, but she told me that you can’t have both.
I understand that the treatments are the same, but I’ve become frustrated with the rheumatologist describing these flare-ups as if they’re nothing more than moans about normal everyday pains suffered by the general population. Can you have both? Does palindromic rheumatism continue alongside rheumatoid arthritis or morph into it?
Susan, via email – 2015
A) Really interesting question, thank you. Palindromic rheumatism is a challenging condition to live with and to diagnose. But from what you describe in your email it does sound as though you currently have rheumatoid arthritis with flare-ups, rather than palindromic rheumatism.
One of the big differences between the two conditions is that you don’t usually see joint damage in palindromic rheumatism.
Read Also: Restore Sql Database From Bak File